Abstract
Second allogeneic stem cell transplantation (alloSCT2) is an increasingly used treatment for acute myeloid leukemia relapsing after first alloSCT. The scope of this study was to analyze trends in patient characteristics, transplant settings and outcome over time to identify factors associated with improved results after alloSCT2.
In this retrospective registry-based analysis, 1540 patients receiving a second alloSCT after hematologic relapse between 2000 and 2019 were included, excluding alloSCT2 given for graft failure. Patients were grouped by period of transplant in 5-year intervals, median follow-up from alloSCT2 was 4.9 years. Over time, the number of patients reported to have received an alloSCT2 in EBMT centers increased from 144 in the period 2000-2004 to 619 in 2015-2019, with remarkable changes with respect to patient characteristic and transplant setting: In recent time periods, patients were of older age (median age 43.4 years between 2000-2004 and 48.6 years between 2015-2019, p=0.012) and had a better performance status before alloSCT2 (2000-2004: Karnofsky index ≥90% in 25.5% patients, 2015-2019: increase to 58.5%, p<0.001). Beyond, the interval between relapse after alloSCT1 and alloSCT2 increased from 2.5 to 3.5 months (p<0.001). In the more recent time periods, a different donor for second alloSCT and especially unrelated [increase from 30.6% (2000-2004) to 61.7% (2015-2019)] and haploidentical [increase from 0.7% (2000-2004) to 22.9% (2015-2019)] donors were used more frequently (p<0.0001 each). Finally, over time more myeloablative conditioning (MAC) (p=0.045), more in vivo T cell depletion (p<0.001), post-transplant cyclophosphamide (p<0.001) and ciclosporin A/MMF for graft versus host disease (GVHD) prophylaxis (p<0.001) were used in alloSCT2.
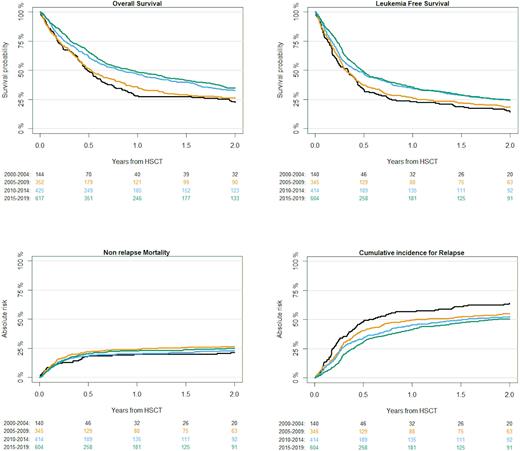
Concerning clinical results after alloSCT2, cumulative relapse incidence (RI) after alloSCT2 decreased over time, whereas outcome improved (Figure 1). Between 2000 and 2019, two-year overall survival (OS) increased from 22.5% to 35%, leukemia free survival (LFS) increased from 14.5% to 24.5%. Whereas no clear trend was observed for incidence of GVHD and non-relapse mortality (NRM), RI decreased from 64% to 50.7%. In multivariate analysis, a later period of alloSCT2 was closely associated with improved OS and LFS (2015-2019: HR 0.47, p<0.001 for OS, HR 0.53, p=0.01 for LFS). Beyond, disease status at alloSCT2 had significant effects on OS, LFS, RI and NRM (HR for active disease at alloSCT2 1.59, p<0.001 for OS; HR 1.63, p<0.001 for LFS; HR 1.91, p<0.001 for RI; HR 1.35, p=0.04 for NRM). Similarly, longer remission duration after alloSCT1 was associated with better OS and LFS, lower RI and higher rates of NRM and acute GVHD (HR for lower remission duration 1.83, p<0.001 for OS; HR 1.72, p<0.001 for LFS; HR 1.86, p<0.001 for RI; HR 1.46, p=0.01 for NRM, HR 1.32, p=0.02 for acute GVHD). AlloSCT2 from haploidentical or unrelated donor, and older patient age were associated with higher NRM (HR 1.88, p=0.01 for haploidentical donor, HR 2.14, p<0.001 for unrelated donor, HR 1.1, p<0.001 for increasing age by 5-year intervals) and therefore inferior OS (HR 1.34, p=0.02 for haploidentical donor, HR 1.32, p=0.02 for unrelated donor, HR 1.05, p=0.002 for age). Further, MAC was associated with decreased RI without increase in NRM, leading to increased OS and LFS (HR 0.7, p<0.001 for RI, HR 1.1, p=0.47 for NRM, HR 0.82, p=0.02 for OS, HR 0.79, p=0.002 for LFS). LFS and OS were positively affected by a better Karnofsky index (HR 0.84, p=0.02 for LFS, HR 0.74, p<0.001 for OS). In vivo T-cell depletion was associated with lower NRM and lower rates of GVHD (HR 0.7, p=0.02 for NRM, HR 0.52, p<0.001 for acute GVHD II-IV, HR 0.64, p=0.003 for chronic GVHD).
In conclusion, according to this large registry analysis on >1500 patients, outcome after alloSCT2 has continuously improved over the last two decades despite increasing patient age. In particular, decreased relapse incidence that did not come at cost of increased toxicity could be observed. This might be a result of better disease control and improved performance score at time of alloSCT2, as well as an increasing use of MAC, in vivo T-cell depletion and eventually post-transplant cyclophosphamide in alloSCT2 over time. These data encourage to perform alloSCT2 in relapsed AML and may help to define future strategies.
Figure Legend
Figure 1: Outcome after alloSCT2
Disclosures
Finke:Riemser Pharma: Research Funding. Kröger:Takeda: Consultancy, Honoraria; Sanofi: Honoraria; Kite: Honoraria; Neovii: Honoraria, Research Funding; Riemser: Research Funding; DKMS: Research Funding; Amgen: Honoraria; BMS: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Jazz: Honoraria. Stelljes:Jazz: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; MSD: Consultancy, Honoraria; Amgen: Consultancy; BMS: Consultancy, Honoraria; Kite: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria, Research Funding; Medac: Honoraria. Dreger:Novartis: Honoraria; Kite: Honoraria. Schmid:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Kite: Research Funding; Abbvie: Research Funding. Ciceri:Kite Pharma: Consultancy. Mohty:Novartis: Honoraria; Astellas: Honoraria; Jazz Pharmaceuticals: Honoraria, Research Funding; Amgen: Honoraria; Takeda: Honoraria; Bristol Myers Squibb: Honoraria; Celgene: Honoraria; Adaptive Biotechnologies: Honoraria; Oncopeptides: Honoraria; Pfizer,: Honoraria; GSK: Honoraria; Sanofi: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Gilead: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal